Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Trauma: Cardiac Arrest
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Initial Trauma Assessment and Management |Thoracic Trauma Assessment and Management |Flail Chest Rib fractures |Resuscitative Thoracotomy |Haemorrhage control |Traumatic Head/Brain Injury |Traumatic Cardiac Arrest |Abdominal trauma |Tranexamic Acid |Silver Trauma |Cauda Equina |Spinal Cord Anatomy |Initial Trauma Assessment and Management |Cervical Spine Immobilization and Management |Anatomy of the Cervical Vertebrae C1 (Atlas) and C2 (Axis) |Trauma: Spinal Injury
Introduction
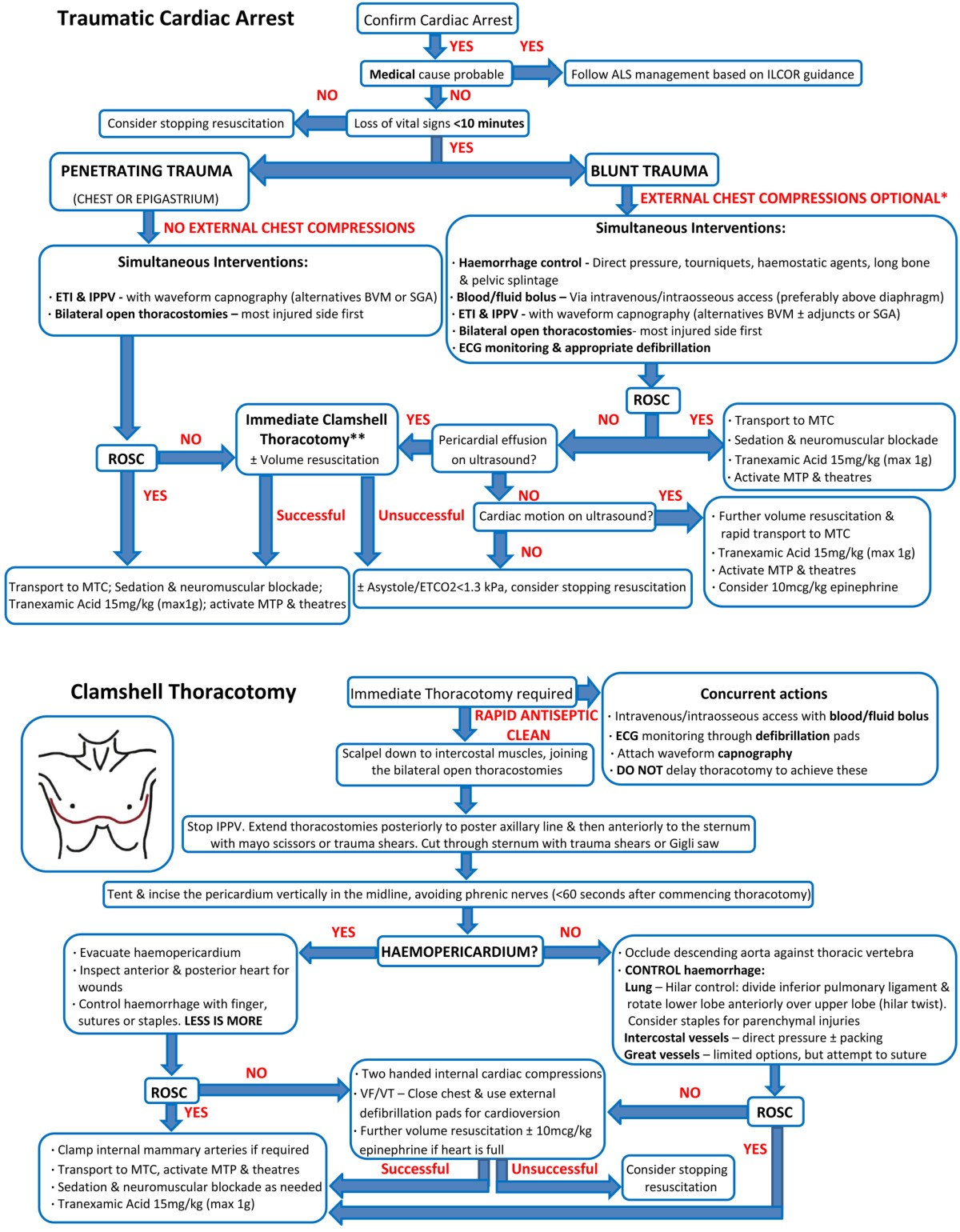
🚨 Trauma-related cardiac arrest (TRCA) is a critical emergency where the heart stops effectively due to severe injury. Unlike medical cardiac arrest, TRCA usually has reversible mechanical or physiological causes (bleeding, hypoxia, tamponade) and requires a targeted trauma approach rather than standard ACLS.
Causes
- 🩸 Hypovolemia: severe internal/external haemorrhage.
- 🫁 Tension pneumothorax: lung collapse with mediastinal shift.
- 💔 Cardiac tamponade: pericardial blood/fluid compressing the heart.
- 🌬️ Hypoxia: airway obstruction or respiratory failure.
- 🫀 Massive PE: rare but possible after trauma.
- ❄️ Hypothermia: low core temperature impairs contractility.
Pathophysiology
Most TRCAs stem from 🩸 haemorrhagic shock → preload failure → PEA. Obstructive causes (tamponade, tension pneumothorax) prevent filling. 🌬️ Hypoxia worsens cellular dysfunction, precipitating arrest.
Assessment (ATLS framework)
- 🅰️ Airway: patency, C-spine control.
- 🅱️ Breathing: chest movement, auscultation, needle decompression if suspected tension.
- 🅲️ Circulation: pulses, haemorrhage control, IV/IO access.
- 🅳️ Disability: GCS, pupillary response.
- 🅴 Exposure: identify injuries, prevent hypothermia.
Management Principles
🏥 Key difference from medical arrest: Fix the cause (bleeding, tamponade, pneumothorax) rather than prolonged CPR + drugs. Chest compressions are adjunctive, not definitive.
Immediate Actions
- ⚠️ Scene safety and activate trauma team.
- 🤝 Call surgical/cardiothoracic backup early.
- 💨 Airway: intubate if indicated, give 100% O₂.
- ❤️ Start compressions only if no cardiac output.
- 🔎 Use POCUS/eFAST to check cardiac activity, tamponade, pneumothorax, bleeding.
Treating Reversible Causes
- 🩸 Hypovolemia: direct pressure/tourniquets, pelvic binder, TXA, MHP (1:1:1 RBC:plasma:platelets).
- 🫁 Tension pneumothorax: needle decompression ➝ chest tube.
- 💔 Tamponade: pericardiocentesis (temporary) ➝ resuscitative thoracotomy.
- 🌬️ Hypoxia: airway clearance, intubation, ventilation.
- ❄️ Hypothermia: warm blankets, warmed IV fluids, heated oxygen.
Adjuncts
- 🖥️ Ultrasound: assess cardiac motion (if none, prognosis poor).
- ⚡ Defibrillate if VF/VT present (rare in TRCA).
- 💊 Drugs: limited role—focus on surgical/trauma fixes.
Special Considerations
- 🔪 Resuscitative Thoracotomy: Indicated for penetrating thoracic trauma with signs of life in ED. Allows tamponade release, cardiac massage, aortic cross-clamp.
- ⏹️ Termination: Blunt trauma arrest without signs of life and no ROSC after reversible causes addressed → cease efforts (per ERC/RCEM guidance).
Prognosis
📉 Overall survival is < 5%. 🔪 Penetrating trauma (esp. cardiac stab wounds) → best outcomes. 🚗 Blunt trauma arrest → survival is extremely rare.
Conclusion
TRCA requires rapid recognition and immediate treatment of reversible causes. 💡 Unlike medical cardiac arrest, the emphasis is surgical: haemorrhage control, decompression, thoracotomy. Outcome depends on mechanism—penetrating > blunt.
References
- ATLS 10th Ed. American College of Surgeons, 2018.
- Soar J, Nolan JP, Böttiger BW, et al. ERC Guidelines, 2021.
- Hopson LR, Hirsh E, Delgado J, et al. J Am Coll Surg 2003;196(1):106-112.