Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Trauma: Resuscitative Thoracotomy
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Initial Trauma Assessment and Management |Thoracic Trauma Assessment and Management |Flail Chest Rib fractures |Resuscitative Thoracotomy |Haemorrhage control |Traumatic Head/Brain Injury |Traumatic Cardiac Arrest |Abdominal trauma |Tranexamic Acid |Silver Trauma |Cauda Equina |Adult Resus:Basic Life Support |Adult Resus: Advanced Life Support |Resus:Acute Haemorrhage
Introduction
- 🫀 Resuscitative thoracotomy is a last-resort, life-saving procedure in catastrophic trauma, performed to restore circulation and control exsanguination.
- It should only be undertaken by trained and credentialed professionals (Emergency Physicians, trauma surgeons, cardiothoracic surgeons) in centres equipped for definitive care.
- ⚡ While ideally performed in theatre, if a patient loses cardiac output it must be carried out immediately in the Emergency Department.
Indications
🎯 Primary goals: relieve tamponade, decompress tension, control haemorrhage, restore circulation.
- 💨 Decompression of tension pneumothorax
- ❤️ Relief of pericardial tamponade
- 🪡 Repair of penetrating cardiac wounds
- 🩸 Control of intrathoracic haemorrhage
- ✋ Open cardiac massage
- 🔑 RCEM: within the scope of practice for trained Emergency Physicians in extremis.
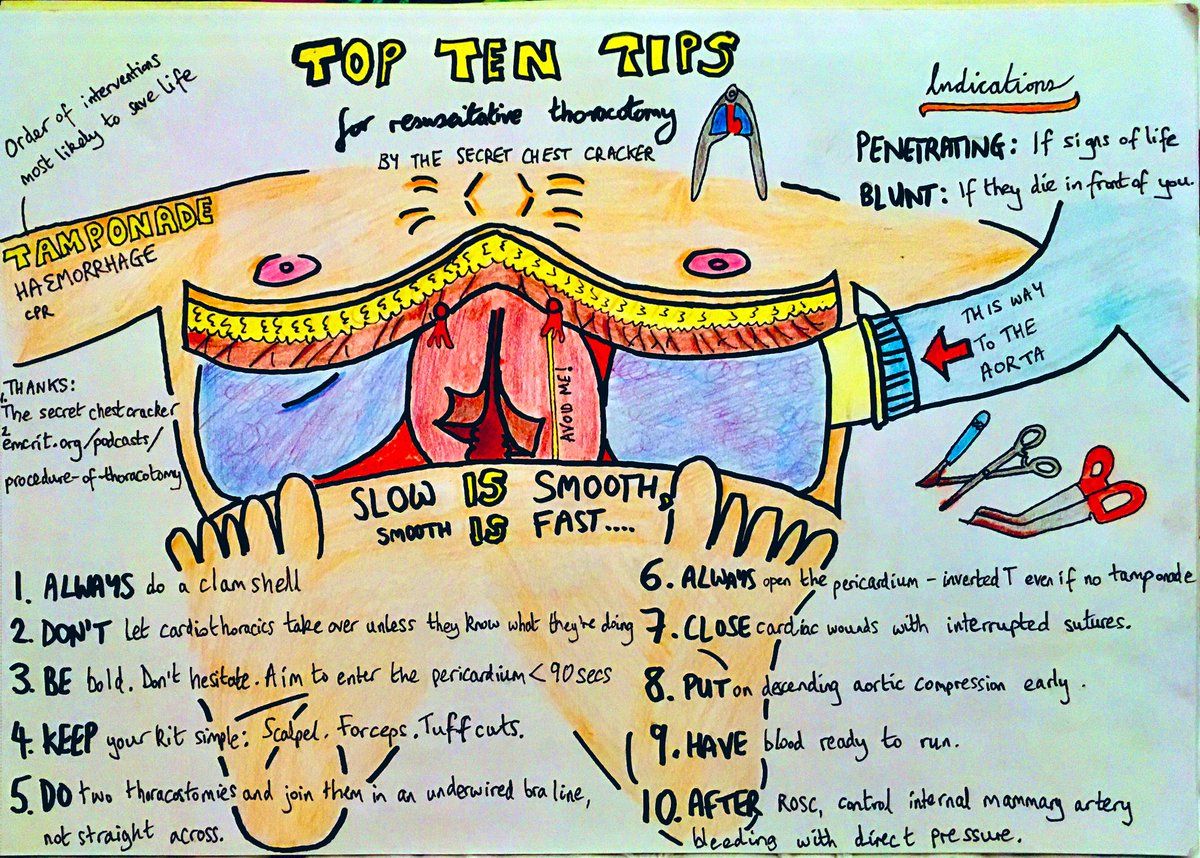
✅ Absolute Indications: - Penetrating chest trauma with witnessed loss of output in ED. - Tamponade with cardiac arrest. - Exsanguinating thoracic haemorrhage.
❌ Contraindications: - No cardiac output for >10 mins without ROSC. - Asystole without pericardial tamponade. - Blunt trauma with cardiac arrest (unless tamponade strongly suspected).
Acute Management Protocol
- 📞 Call cardiothoracic support – notify consultant + SpR immediately.
- 🧰 Prepare thoracotomy kit – sterile instruments, suction, lighting, cardiac sutures.
- 🔍 Indications check – penetrating thoracic/upper abdominal trauma with arrest, or need for aortic cross-clamp in exsanguination.
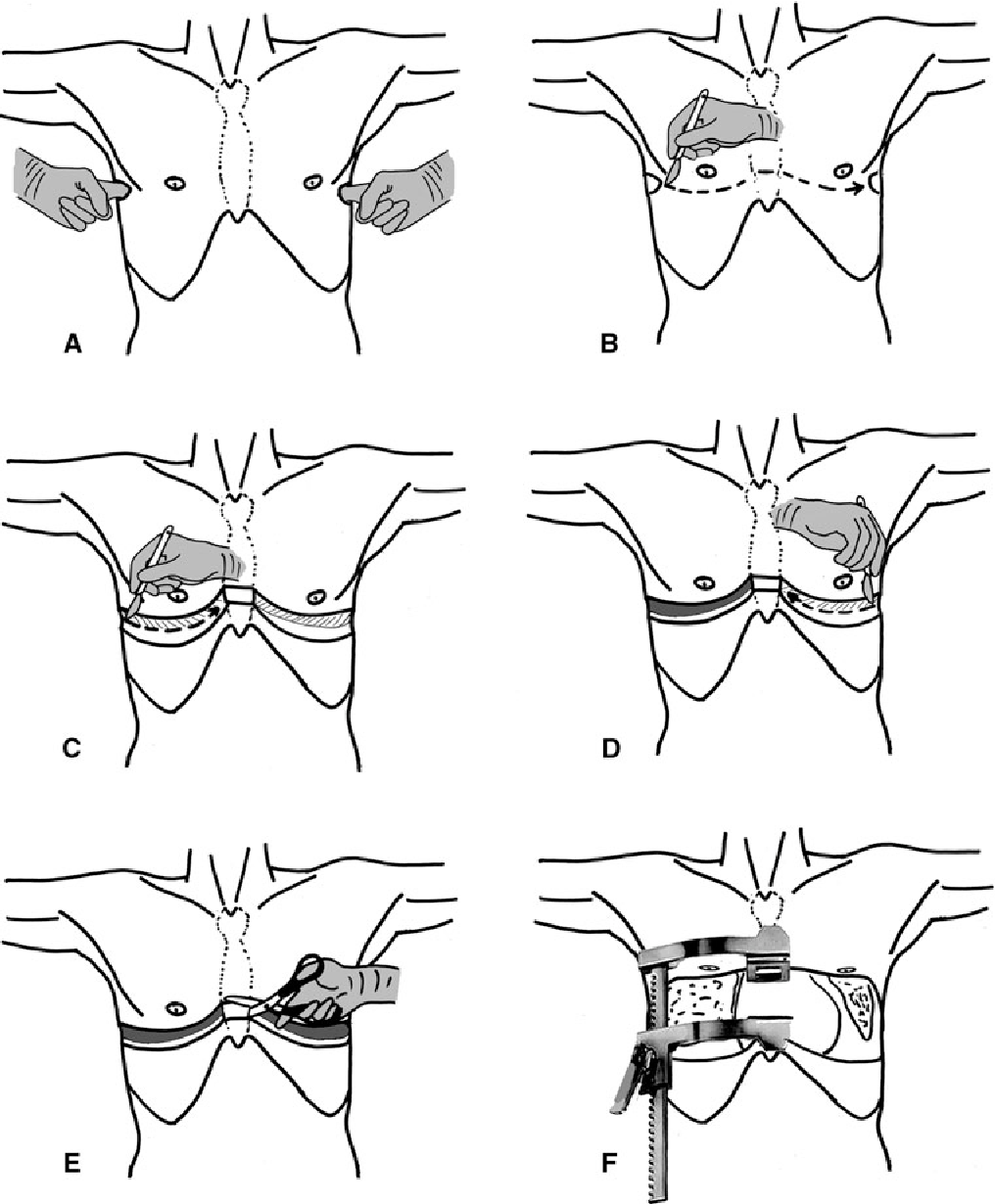
- ✂️ Bilateral thoracostomies – 5th intercostal space, mid-axillary line; decompress air/fluid before proceeding.
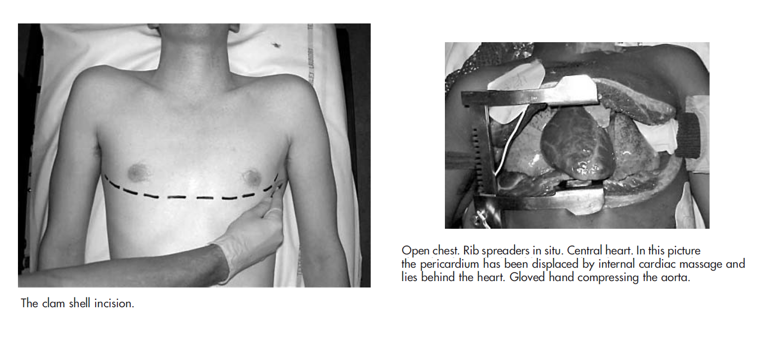
- 🔪 Clamshell incision – join thoracostomies across sternum (Tuff Cut scissors / Gigli saw).
- 🫀 Cardiac/pericardial management:
- Open pericardium longitudinally; evacuate blood/clot.
- Direct pressure or 4-0 Prolene sutures for cardiac wounds.
- Pack/Foley catheter for temporary tamponade.
- ⛓️ Control bleeding – clamp hilum/aorta if required.
- 🤲 Open cardiac massage if no spontaneous output.
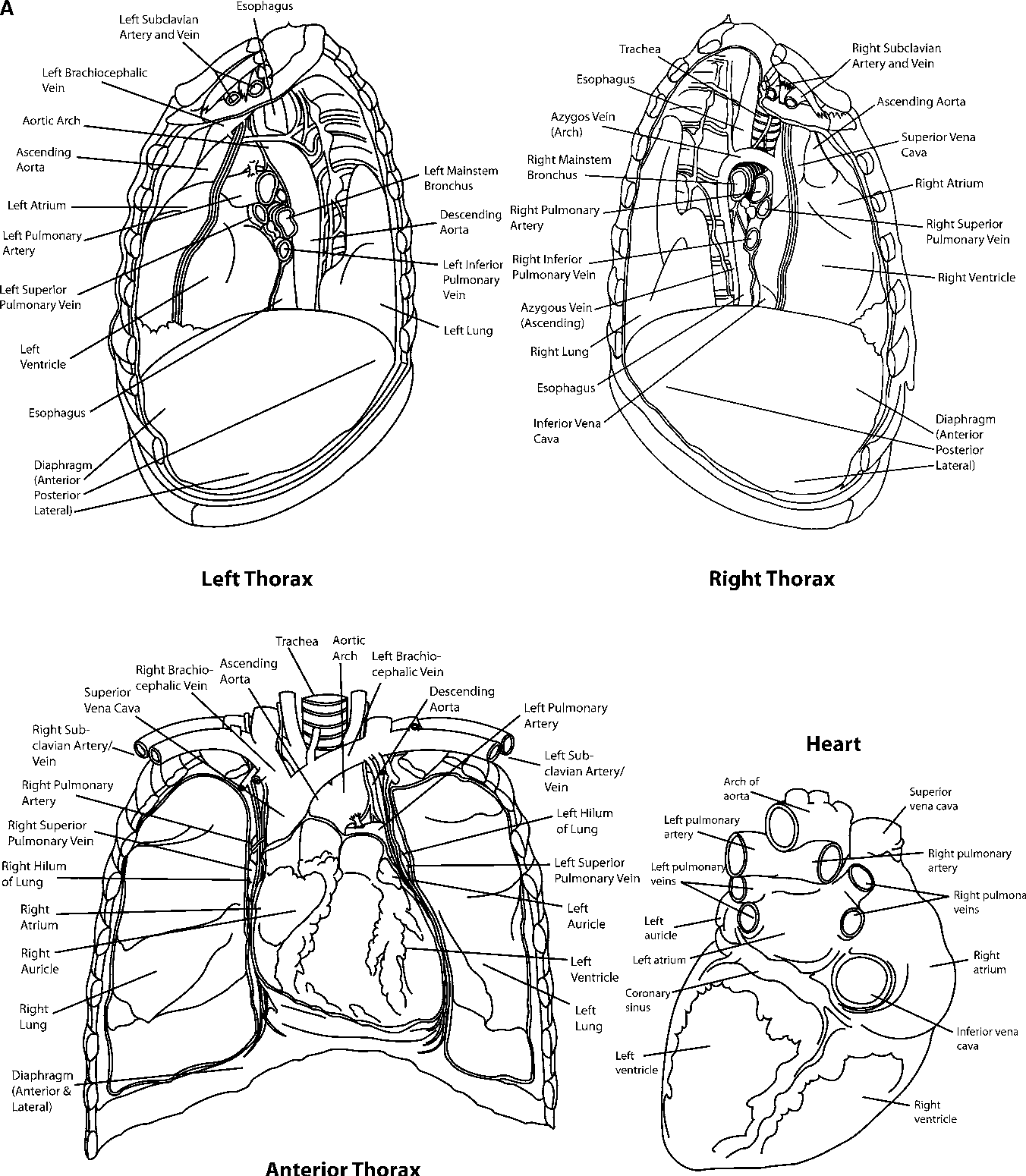
Relevant Anatomy
- ❤️ Heart + great vessels (aorta, pulmonary arteries, SVC/IVC)
- 🫁 Lungs & pleura (managing haemothorax/pneumothorax)
- 🪶 Diaphragm (injuries may extend to abdomen)
Surgical Approaches
- 🟧 Clamshell incision – gold standard ED approach; excellent bilateral access.
- 🟥 Left anterolateral thoracotomy – faster, for left-sided/cardiac access.
- ⬜ Median sternotomy – ideal in controlled theatre settings.
Post-Procedure Considerations
- 🩺 Stabilisation – haemostasis, volume resuscitation, secure airway/ventilation.
- 📉 Monitoring – haemodynamics, arrhythmias, re-bleeding.
- 📝 Documentation – timings, interventions, findings, patient response.
- 🚑 Transfer – to operating theatre or ICU for definitive management.
Outcomes
- 🔪 Penetrating cardiac trauma – survival up to 15–20% if performed promptly.
- 🚗 Blunt trauma – survival extremely poor (<2%).
- ⏱️ Outcome depends on time to thoracotomy, mechanism of injury, and availability of definitive surgical repair.
References
- Royal College of Emergency Medicine (RCEM) Guidelines
- NEJM Review: Resuscitative Thoracotomy
- Advanced Trauma Life Support (ATLS®) 10th Edition