Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Stroke Penumbra
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Hypertension |Mechanical Thrombectomy |Stroke Penumbra |Cardiac Thrombolysis |Stroke Thrombolysis |Alteplase |Tenecteplase |Streptokinase |Reteplase
Understanding the Stroke Penumbra
The stroke penumbra is a critical region of brain tissue that lies just beyond the core area affected by an ischaemic stroke. Unlike the core, where cells are irreversibly damaged due to a severe lack of blood flow, the penumbra contains cells that are at serious risk but may still be salvageable with timely intervention.
Within the first few hours after a stroke occurs, the penumbral tissue remains in a vulnerable state. Blood flow in this area is significantly reduced, typically between 30-50% of normal perfusion levels, leading to hypoxia and energy failure in neurons. However, this reduced blood flow does not immediately result in cell death. By restoring circulation and providing appropriate medical treatments, it is possible to rescue these cells, thereby reducing overall neurological damage and improving patient outcomes.
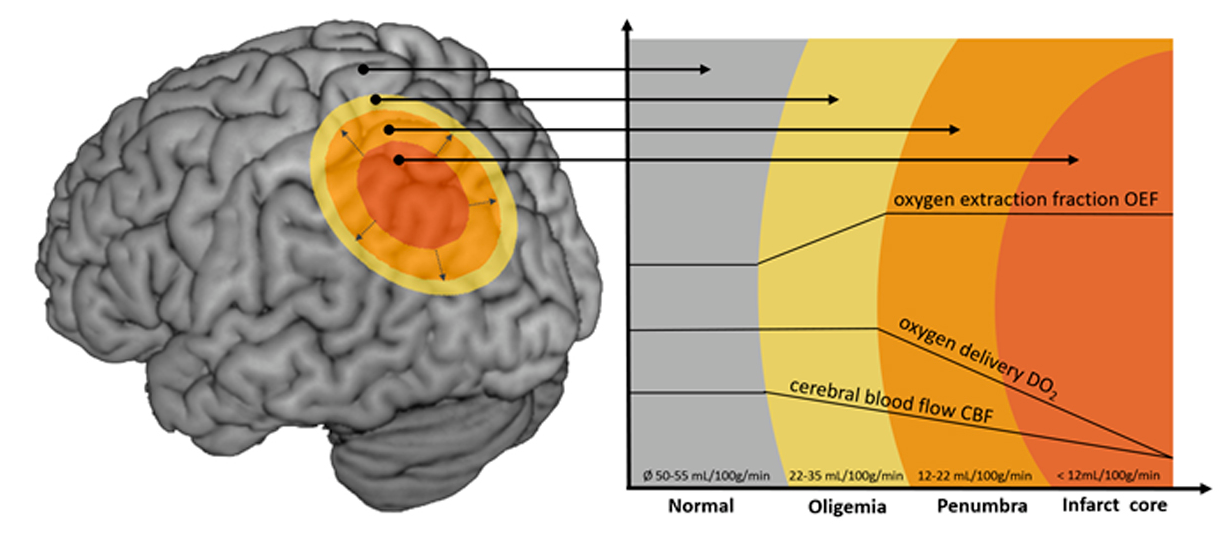
- Key Characteristic: Reduced but not completely halted blood flow, typically 30-50% of normal perfusion.
- Treatment Window: Early intervention, ideally within the first 4.5 hours for thrombolysis and up to 24 hours for endovascular therapy, is crucial to prevent irreversible tissue loss.
- Imaging Importance: Advanced imaging techniques such as MRI perfusion and CT perfusion are essential for identifying the penumbra and guiding targeted therapy.
Identifying and treating the penumbra is central to modern stroke management strategies. The goal is to administer therapies—such as intravenous thrombolytics or endovascular treatments—within the critical time window, thereby improving patient outcomes and preserving as much brain function as possible.
Pathophysiology
- Ischaemic Core: The area with critically reduced blood flow (<30% of normal), leading to rapid and irreversible neuronal death.
- Penumbral Tissue: Surrounding area with moderately reduced blood flow (30-50% of normal), where neurons are dysfunctional but not yet dead.
- Inflammatory Response: In the penumbra, inflammation can exacerbate injury if not controlled.
- Excitotoxicity: Excess glutamate release in the penumbra contributes to neuronal injury and death.
Importance of Time in Stroke
- Time is Brain: Approximately 1.9 million neurons are lost each minute during an untreated stroke.
- Golden Hour: The first hour after stroke onset is critical for maximizing treatment efficacy.
- Time-Dependent Therapies: Intravenous thrombolysis is most effective within 4.5 hours, while mechanical thrombectomy can be beneficial up to 24 hours in selected patients.
Imaging Techniques
- CT Perfusion: Assesses blood flow, volume, and transit time to differentiate between core and penumbral tissue.
- MR Perfusion: Provides detailed images of cerebral blood flow and helps identify salvageable brain tissue.
- Diffusion-Weighted MRI: Identifies areas of restricted diffusion, indicating the core of the stroke.
- Perfusion-Weighted MRI: Visualizes the penumbra by showing areas with reduced perfusion but still viable tissue.
Treatment Modalities
- Intravenous Thrombolysis: Administration of tissue plasminogen activator (tPA) to dissolve the clot and restore blood flow.
- Mechanical Thrombectomy: Endovascular procedure to physically remove the clot from the blocked artery.
- Neuroprotective Agents: Medications aimed at protecting penumbral neurons from further damage.
- Supportive Care: Includes maintaining airway, breathing, and circulation (ABCs), managing blood pressure, and preventing complications.
Prognosis
- Early treatment can significantly improve functional outcomes and reduce mortality rates.
- Extent of penumbral tissue salvage correlates with better neurological recovery.
- Delayed treatment increases the risk of extensive brain damage and long-term disability.
- Rehabilitation services are essential for maximizing recovery post-stroke.
Conclusion
- The stroke penumbra represents a critical target for intervention in ischaemic stroke.
- Timely identification and treatment of the penumbra can prevent irreversible brain damage and improve patient outcomes.
- Advancements in imaging techniques have enhanced the ability to detect the penumbra, facilitating more effective and personalized treatment approaches.