Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Mechanical Thrombectomy for Ischaemic Stroke
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Hypertension |Mechanical Thrombectomy |Stroke Penumbra |Cardiac Thrombolysis |Stroke Thrombolysis |Alteplase |Tenecteplase |Streptokinase |Reteplase
🧠 Mechanical thrombectomy is a life-saving endovascular procedure used to remove large clots from cerebral arteries in acute ischemic stroke. ⚡ It has revolutionized stroke care by rapidly restoring blood flow, improving survival, and reducing long-term disability when performed promptly.
📖 About
- Definition: Endovascular removal of intracranial clots in large vessel occlusion (LVO) stroke.
- History: Modern thrombectomy emerged in 2015 with stent retrievers & aspiration catheters after multiple landmark RCTs.
- Purpose: Rapid recanalization → salvage brain tissue → improve functional outcome.
📑 Evidence & Number Needed to Treat (NNT)
- Landmark RCTs:
- MR CLEAN, ESCAPE, REVASCAT, SWIFT PRIME, EXTEND-IA → all showed clear benefit over IV thrombolysis alone.
- Meta-analyses: Confirm thrombectomy is superior to medical therapy alone for LVO strokes.
- NNT:
- ~2–3 to achieve functional independence (mRS 0–2 at 90 days).
- ~6–10 to prevent one death.
- Guidelines: AHA, ESO & NICE endorse thrombectomy for eligible patients.
🧾 Pre-Thrombectomy Assessment
- Clinical: NIHSS to quantify deficit severity (higher scores suggest LVO).
- Imaging:
- NCCT: exclude haemorrhage.
- CTA: confirm large vessel occlusion.
- CTP/MR perfusion: assess penumbra vs infarct core.
- Labs: FBC, coagulation profile, renal function (contrast safety), glucose.
- Eligibility:
- Time window: ≤6h (up to 24h in selected patients by perfusion imaging).
- LVO: ICA, MCA (M1/M2), basilar artery.
- Adequate salvageable brain tissue.
- No major contraindications (extensive infarct, severe comorbidity).
🎯 Indications
- Acute ischemic stroke with confirmed LVO.
- Within time window (6–24h depending on imaging).
- Favourable penumbra-to-core ratio on perfusion studies.
🛠️ Devices
- Stent Retrievers: Solitaire, Trevo → ensnare clot & pull it out.
- Aspiration Catheters: ADAPT → suction clot out.
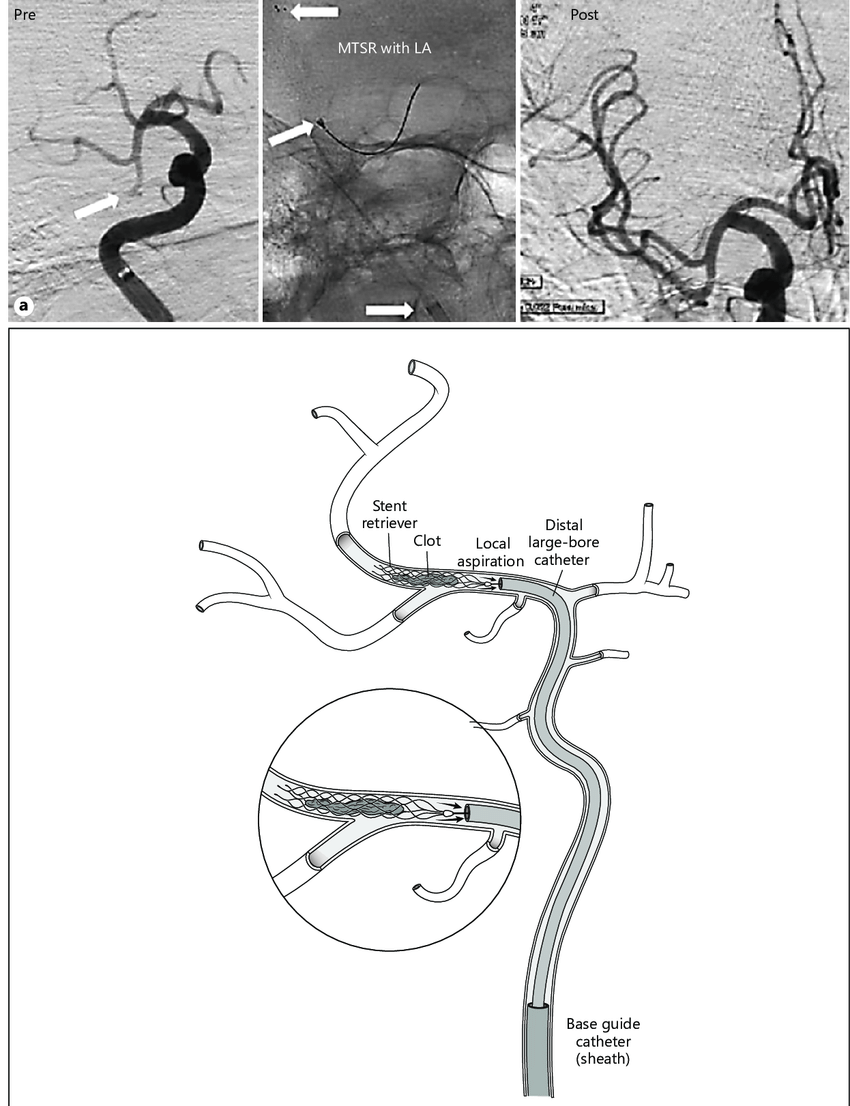
- Combined Techniques: Stent retriever + aspiration (Solumbra approach).
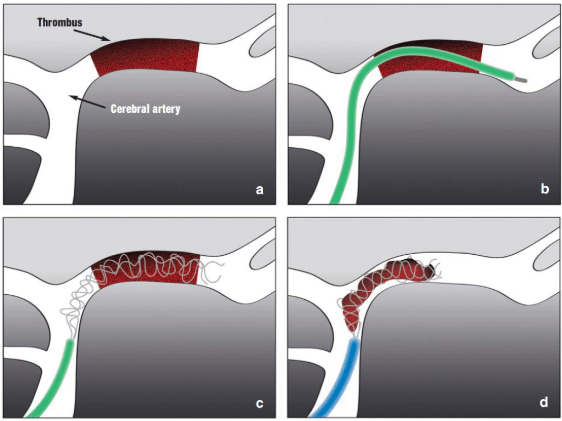
⚙️ Procedure
- Access: Usually femoral artery → navigate catheter to clot.
- Retrieval: Deploy retriever/aspiration → remove clot (multiple passes if needed).
- Verification: Angiography confirms recanalization (TICI 2b–3 = success).
- Closure: Sheath removal & haemostasis.
⚠️ Complications
- Intracranial haemorrhage (ICH).
- Vessel injury: dissection or perforation.
- Distal embolization of clot fragments.
- Access site haematoma/AV fistula.
- Reperfusion injury.
- Contrast nephropathy (rare).
📈 Outcomes
- Recanalization success in >80–90% with modern devices.
- Significant functional improvement (mRS 0–2 at 90 days in 45–60%).
- Mortality reduction compared to IV thrombolysis alone.
- “Time is brain”: benefit falls with delay.
🩺 Post-Procedure Care
- ICU/HDU monitoring for neuro status & haemodynamics.
- Follow-up CT/MRI to assess reperfusion & exclude haemorrhage.
- Early rehabilitation: physio, OT, speech therapy.
- Secondary prevention: antiplatelet/anticoagulation as indicated.
🚀 Recent Advances
- Better imaging → extended treatment windows (DAWN, DEFUSE 3 trials).
- Next-gen aspiration catheters with improved suction.
- Trials of posterior circulation thrombectomy (basilar artery occlusion).
✅ Conclusion
Mechanical thrombectomy is now gold standard therapy for eligible LVO strokes. Success depends on rapid recognition, efficient pathways, expert intervention, and careful post-stroke care. Each minute saved → better neurological recovery.
📚 References
- Goyal M, Menon BK, et al. Lancet 2016;387:1723–31.
- Albers GW, Marks MP, et al. NEJM 2018;378:708–18.
- NINDS – Mechanical Thrombectomy
- World Stroke Organization – Guidelines