Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Fetal-type Posterior cerebral artery (FTP)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
🧠 The presence of a fetal-type Posterior Cerebral Artery (PCA) can significantly influence cerebral blood flow dynamics — especially during ischaemic events. In this variant, the posterior circulation becomes partly or wholly dependent on the internal carotid artery (ICA). Thus, if an ischaemic event affects the ICA, perfusion may be reduced not only to the anterior (ACA, MCA) but also to the posterior cerebral territories (occipital lobes). Most people remain asymptomatic, but this variant can predispose to posterior TIAs or occipital strokes in the setting of carotid artery disease. ⚠️
🧩 About
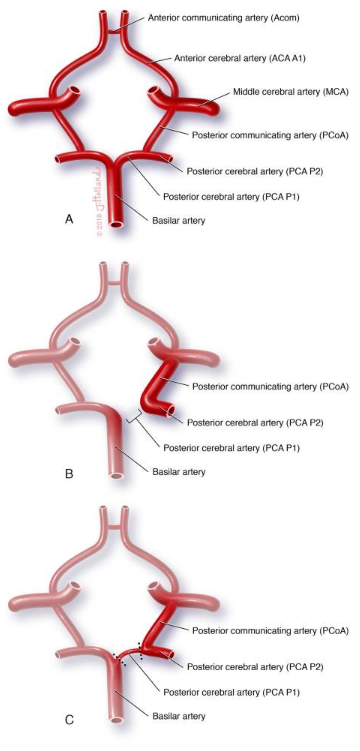
- The fetal posterior cerebral artery (PCA) is a developmental vascular variant in which the PCA arises directly from the internal carotid artery instead of the basilar artery.
- This reflects persistence of the fetal circulation pattern — when anterior and posterior circulations are more closely linked.
- Normally, the PCA is supplied by the basilar artery via the P1 segment. In the fetal variant, the PCA originates from the carotid via an enlarged posterior communicating artery (PComA).
- May be unilateral or bilateral and occasionally partial (a “transitional” variant where both the ICA and basilar supply the PCA).
📊 Incidence
- Occurs in roughly 4–29% of individuals depending on the study and imaging technique used.
- Slightly more common unilaterally (left more than right).
- Persistence into adulthood reflects developmental variation rather than pathology.
🧠 Clinical Relevance
- ⚡ Ischaemic Impact: The fetal PCA changes the usual collateral routes within the Circle of Willis. If the ICA is blocked, both anterior and posterior cerebral areas can become ischaemic, producing mixed cortical deficits (e.g. combined visual + motor/sensory symptoms).
- 😌 Asymptomatic in Most: Most individuals are unaware of the variant — it’s usually found incidentally on MRI or CTA performed for headaches, dizziness, or unrelated reasons.
- 🫀 Carotid Artery Disease Risk: In patients with carotid stenosis or atherosclerosis, a fetal PCA can increase vulnerability to posterior ischaemia (visual field defects, occipital infarcts).
- 🧩 Implications for Stroke Intervention: Knowledge of a fetal PCA is important in carotid endarterectomy, carotid stenting, or mechanical thrombectomy, as emboli from the ICA may affect posterior circulation territories.
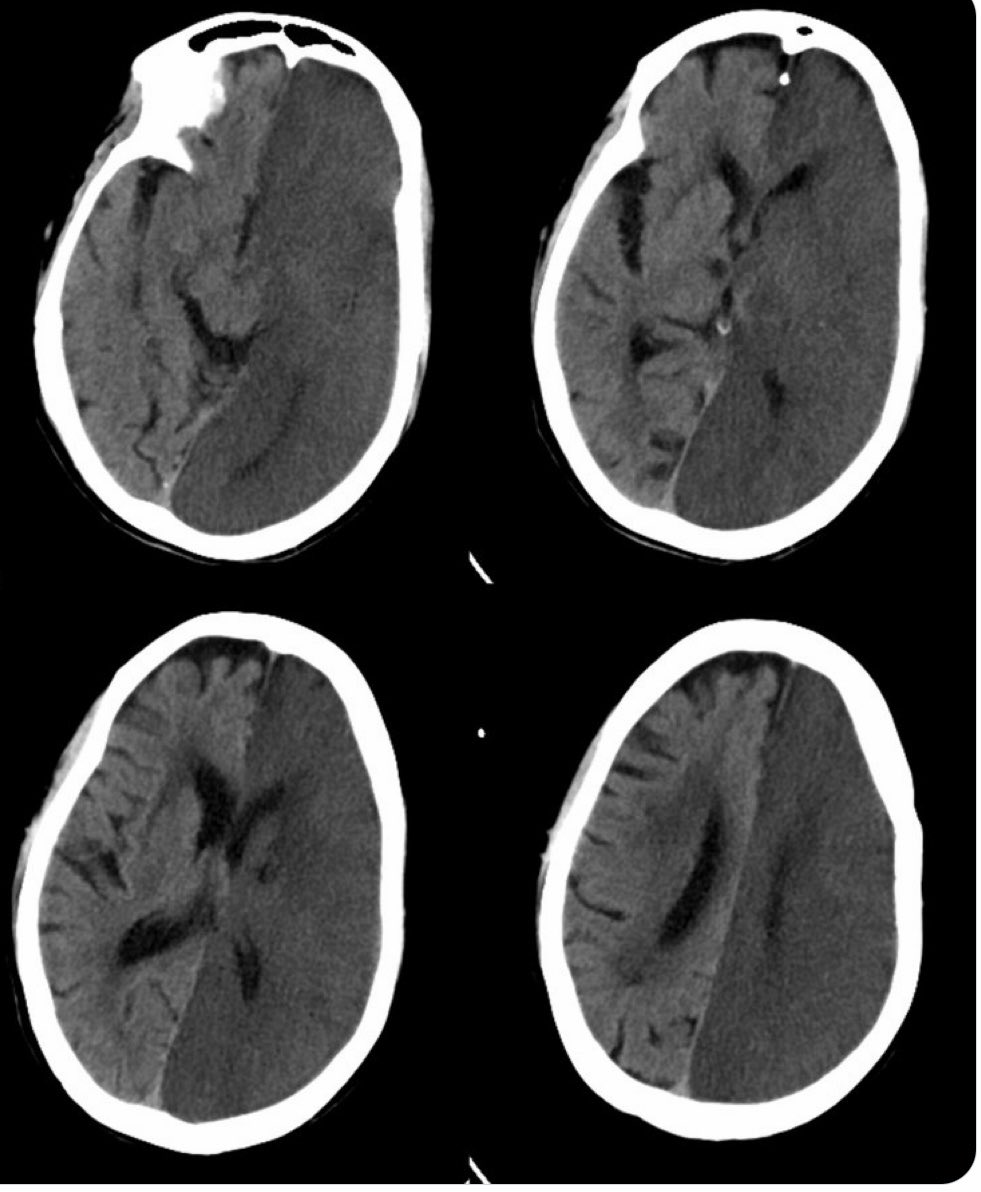
🩸 The image shows the effect of a blocked left internal carotid artery (ICA) — which supplies the MCA, ACA, and a fetal-origin PCA — illustrating how an ICA event can impair both anterior and posterior perfusion territories. This unique pattern highlights the importance of recognising vascular variants in stroke imaging.
🔬 Variants of the Circle of Willis
🧠 In a complete Circle of Willis, the basilar artery connects with the carotid system via a small PComA. In the fetal-type PCA:
- ➡️ Fetal-type PComA: Hypoplastic or absent P1 segment of PCA; PCA supplied predominantly by ICA.
- ➡️ True Fetal PCA: Complete absence of P1 segment — PCA arises entirely from ICA (no basilar connection).
- ➡️ Transitional type: Both ICA and basilar arteries contribute variably to PCA flow.
🧭 Diagnosis
- 🧲 Magnetic Resonance Angiography (MRA): Non-invasive, visualises cerebral blood flow and vessel origins; can identify whether the PCA arises from ICA.
- 🖥️ Computed Tomography Angiography (CTA): Produces detailed vascular mapping — crucial before neurointerventional procedures.
- 💉 Digital Subtraction Angiography (DSA): The gold standard for defining cerebral arterial anatomy when intervention or embolic source localisation is required.
🩺 Management & Clinical Approach
- 🧘♂️ Incidental Finding: Usually requires no intervention if the patient is asymptomatic.
- 🧍♂️ Vascular Risk Optimisation: In patients with carotid disease, hypertension, or diabetes, aggressive vascular risk control is essential (BP, lipid, and glucose management).
- 💊 Antiplatelet Therapy: Considered if other cerebrovascular risk factors are present to prevent thromboembolic events.
- 🧠 Imaging Surveillance: Periodic vascular imaging if associated with carotid stenosis or symptoms suggesting posterior TIAs.
- 🚨 Stroke Prevention: Lifestyle modification — stop smoking, reduce alcohol, maintain exercise and diet — remains cornerstone management.
📚 References
- 🧬 A Fetal-type Variant Posterior Communicating Artery and its Clinical Significance
- Osborn AG. Diagnostic Cerebral Angiography, 2nd ed. Lippincott Williams & Wilkins, 2018.
- van Raamt AF et al., AJNR 2006;27(6):1341–1347 — “Variations in the Circle of Willis.”
💡 Teaching tip: Remember that a fetal PCA converts the posterior circulation into a “carotid-dependent zone.” So in carotid occlusion → think visual symptoms too (homonymous hemianopia). Always review vascular anatomy on MRA/CTA before attributing stroke localisation. 🧠✨