Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
CT Basics for Stroke
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Acute Stroke Assessment (ROSIER&NIHSS) |Atrial Fibrillation |Atrial Myxoma |Causes of Stroke |Ischaemic Stroke |Cancer and Stroke |Cardioembolic stroke |CT Basics for Stroke |Endocarditis and Stroke |Haemorrhagic Stroke |Stroke Thrombolysis |Hyperacute Stroke Care
🧠 Introduction
- 💡 Stroke medicine evolved rapidly with the introduction of CT scanning, enabling clinicians to distinguish between ischaemic and haemorrhagic strokes quickly and safely. Non-contrast CT (NCCT) is the initial investigation of choice for nearly all suspected strokes.
- ⚙️ CT imaging is central to acute stroke management — it determines stroke type, rules out mimics, and guides emergency therapies such as thrombolysis or thrombectomy.
- 📜 Before CT, differentiating stroke subtypes relied on clinical signs or even post-mortem findings. Early diagnostic methods (e.g. pineal calcification displacement) were crude and unreliable.
📚 History of CT Imaging
- 🧑🔬 Sir Godfrey Hounsfield developed the first CT scanner in 1972 — funded by EMI’s Beatles record profits 🎸.
- 🧩 The first clinical CT scan in 1971 (Atkinson Morley Hospital, London) diagnosed a cerebral cyst — a landmark moment in neuroradiology.
- 🏥 By the late 1980s, CT became routine in major hospitals, revolutionising stroke diagnosis and management.
⚙️ Technical Aspects of CT
- 🌀 A CT scanner uses a rotating X-ray tube and detectors to capture cross-sectional images of the body, reconstructed by a computer into slices.
- 🔁 Helical (spiral) CT introduced in the 1990s enabled continuous scanning for 3D reconstructions — essential for vascular imaging.
- 📏 Image density is expressed in Hounsfield Units (HU):
- Air = -1000 HU
- Water = 0 HU
- Grey matter ≈ +35 HU
- Acute haemorrhage ≈ +70 HU
- Bone = +400 to +3000 HU
☢️ Radiation Exposure
- CT involves ionising radiation and is regulated under IRMER in the UK — only to be performed when clinically justified.
- 🧮 A typical CT head ≈ 2 mSv → roughly equivalent to 100 chest X-rays.
- 🌍 Natural background radiation ≈ 3.1 mSv/year for comparison.
| Scan Type | Approx. Radiation Dose (mSv) |
|---|---|
| 🌍 Natural Background | 3.1 / year |
| 🧠 Brain CT | 2.0 |
| 🫁 Chest CT | 7.0 |
| 🫀 Chest + Abdomen + Pelvis | 21.0 |
🏥 CT in Acute Stroke
- CT is first-line for suspected stroke — rules out haemorrhage before thrombolysis or thrombectomy.
- Indications: sudden focal neurological deficit, decreased consciousness, headache, or anticoagulant use.
- ⚠️ Early CT may appear normal within first 6 hours of ischaemia — correlate with clinical findings.
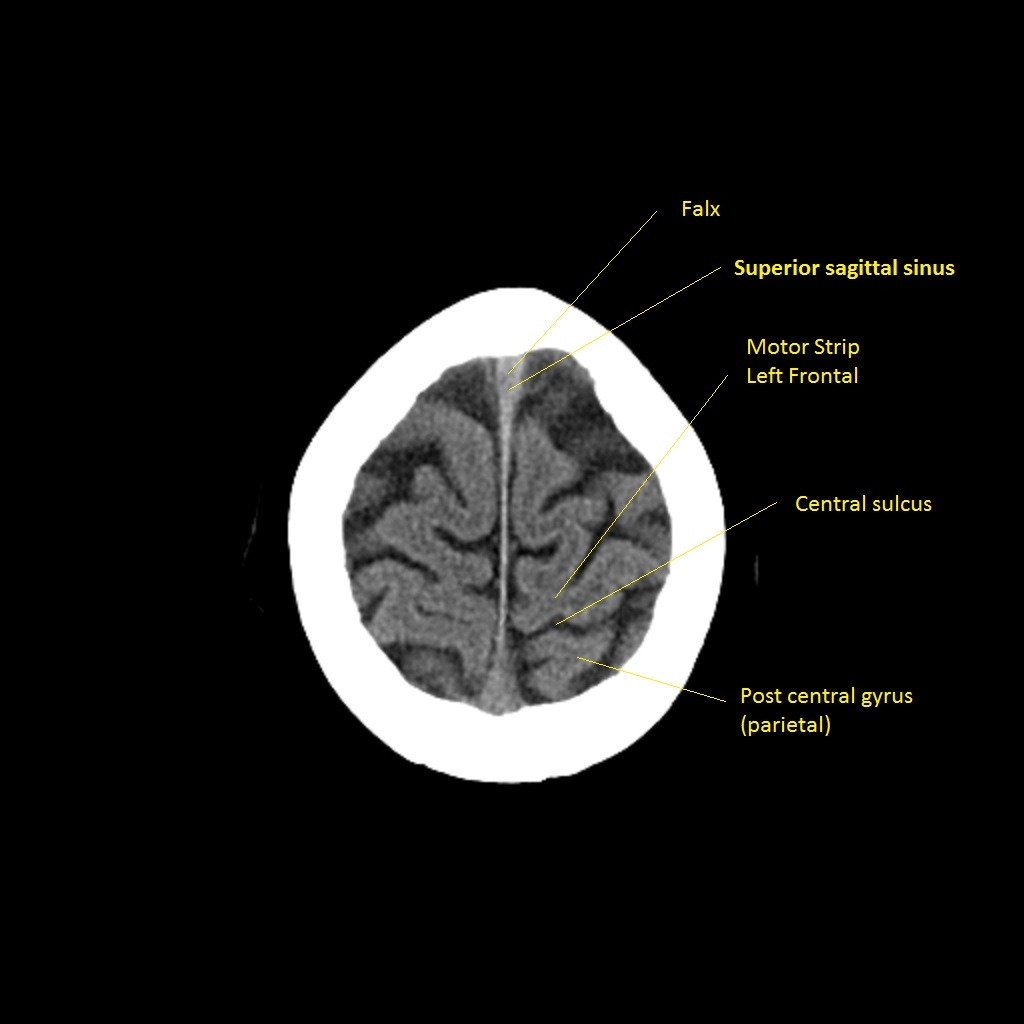
🔍 CT Interpretation Tips
🧩 Review CT systematically from vertex to base. Look for hyperdensities (clots), hypodensities (oedema or infarction), and mass effect. Always exclude mimics such as subdural haematoma or tumour before giving thrombolysis.
🧠 Early Signs of Ischaemia on CT
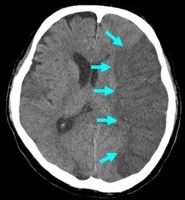
- ⚡ Hyperdense MCA sign: Thrombus in middle cerebral artery — earliest visible clue.
- 🌫️ Loss of grey-white differentiation: Early cytotoxic oedema, especially in cortex or basal ganglia.
- 🌀 Insular ribbon sign: Blurring between insular cortex and adjacent white matter.
- 🌊 Effacement of sulci: Local swelling and oedema flattening cortical grooves.
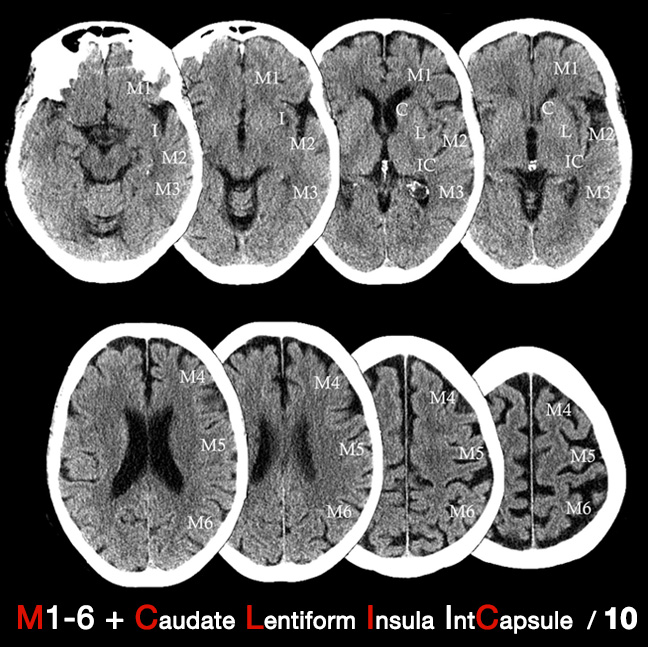
🧮 ASPECTS Score
The Alberta Stroke Program Early CT Score (ASPECTS) assesses early ischaemic change in MCA territory. • Score = 10 (normal), decreasing with extent of infarction. • ASPECTS ≤ 7 → poorer prognosis & higher risk of post-thrombolysis haemorrhage.
🩸 CTA & CT Perfusion (CTP)
- 🧩 CT Angiography (CTA): Maps arteries from aortic arch → Circle of Willis; identifies clots, dissections, or stenosis. Essential before thrombectomy.
- 🎯 CT Perfusion (CTP): Measures blood flow (CBF), volume (CBV), and mean transit time (MTT). Differentiates core infarct vs. penumbra (salvageable tissue).
⚠️ Limitations of CT
- ❌ May miss small brainstem strokes or subtle early cortical ischaemia.
- 🧩 False negatives possible in first few hours; false positives from leukoaraiosis in elderly.
🕓 Later CT Signs (6–24 hours)
- ⬜ Hypodense areas become obvious due to cytotoxic and vasogenic oedema.
- 💔 Haemorrhagic transformation may occur, especially in large infarcts or with anticoagulant use.

💡 Teaching tip: - NCCT remains the first-line scan for stroke — fast, reliable, and accessible. - Subtle early changes demand a trained eye and careful side-by-side comparison. - Combine imaging findings with clinical localisation for accurate decision-making.