Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Anatomy of the Thorax
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Anatomy of Skin |Anatomy of the Hand |Anatomy of the Thorax |Anatomy of Muscle Groups |Anatomy of Arteries |Anatomy of the Spinal Column
🫁 Anatomy of the Thoracic Cavity, Diaphragm, and Lungs
The thoracic cavity forms the central compartment of the human torso, bounded by the thoracic cage and diaphragm. It contains the heart, lungs, great vessels, trachea, and oesophagus — all protected yet mobile enough to permit respiration. Understanding this region underpins interpretation of chest imaging, thoracentesis, cardiac auscultation, and mechanical ventilation in clinical practice.
🏗️ Thoracic Cage Anatomy
The thoracic cage (rib cage) forms a semi-rigid, elastic chamber that protects the thoracic organs while facilitating breathing through rhythmic expansion and recoil. It consists of the sternum anteriorly, 12 pairs of ribs and costal cartilages, and 12 thoracic vertebrae posteriorly.
🩻 Sternum (Breastbone)
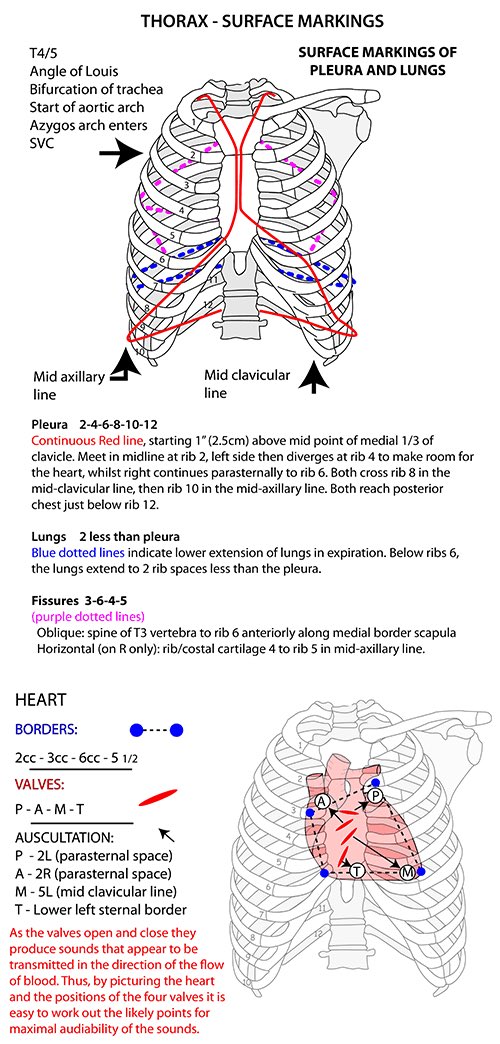
- Manubrium: The superior portion articulates with the clavicles and first two ribs. The jugular notch is palpable between the clavicular heads. The sternal angle (Angle of Louis) marks the T4/T5 level — a critical landmark for locating the 2nd rib, aortic arch, and carina.
- Body (Corpus Sterni): Articulates with ribs 2–7 via costal cartilages and provides attachment to pectoralis major and transversus thoracis muscles.
- Xiphoid Process: The small inferior segment, cartilaginous in youth, ossifies in adults. Serves as an attachment for the diaphragm and rectus abdominis.
🦴 Rib Cage Structure
- True Ribs (1–7): Attach directly to the sternum. Ribs 1 and 2 are atypical, with unique grooves for the subclavian vessels.
- False Ribs (8–10): Attach indirectly via the 7th rib’s cartilage, contributing flexibility.
- Floating Ribs (11–12): Posteriorly attached only; protect kidneys and upper lumbar organs.
Posteriorly, ribs articulate with the vertebral bodies and transverse processes forming costovertebral and costotransverse joints, which allow elevation and depression during breathing.
🔧 Functions of the Thoracic Cage
- Protection: Shields the lungs, heart, and major vessels from mechanical injury.
- Support: Maintains the thoracic framework, anchoring muscles of respiration and upper limb movement.
- Respiration: Elastic cartilages and intercostal muscles enable changes in thoracic volume.
- Haematopoiesis: Sternum and ribs contain red marrow in adults — important for bone marrow aspiration sites.
🫀 Diaphragm Anatomy
The diaphragm is a dome-shaped musculotendinous partition separating thorax and abdomen — the principal muscle of inspiration. It is innervated by the phrenic nerves (C3–C5) — remember “C3,4,5 keep the diaphragm alive”.
- Origins:
- Sternal: posterior xiphoid process.
- Costal: internal surfaces of ribs 7–12.
- Lumbar: right and left crura from L1–L3, joined by median, medial, and lateral arcuate ligaments.
- Openings:
- T8 – Caval opening: Inferior vena cava, right phrenic nerve.
- T10 – Oesophageal hiatus: Oesophagus, vagus nerves.
- T12 – Aortic hiatus: Aorta, thoracic duct, azygos vein.
- Vascular supply: Pericardiophrenic, musculophrenic, and inferior phrenic arteries.
💨 Function
- During inspiration → diaphragm contracts and flattens → thoracic volume ↑ → intrathoracic pressure ↓ → air enters lungs.
- During expiration → diaphragm relaxes → dome rises → pressure ↑ → air expelled.
- Also increases intra-abdominal pressure aiding defaecation, micturition, and childbirth.
🫁 Lung Anatomy
The lungs are paired, conical organs filling most of the thoracic cavity. Their apex extends 2–3 cm above the clavicle, and their base rests on the diaphragm. The right lung is larger but shorter due to the liver beneath it.
- Right Lung: 3 lobes (superior, middle, inferior) separated by horizontal and oblique fissures.
- Left Lung: 2 lobes (superior, inferior), oblique fissure, cardiac notch and lingula.
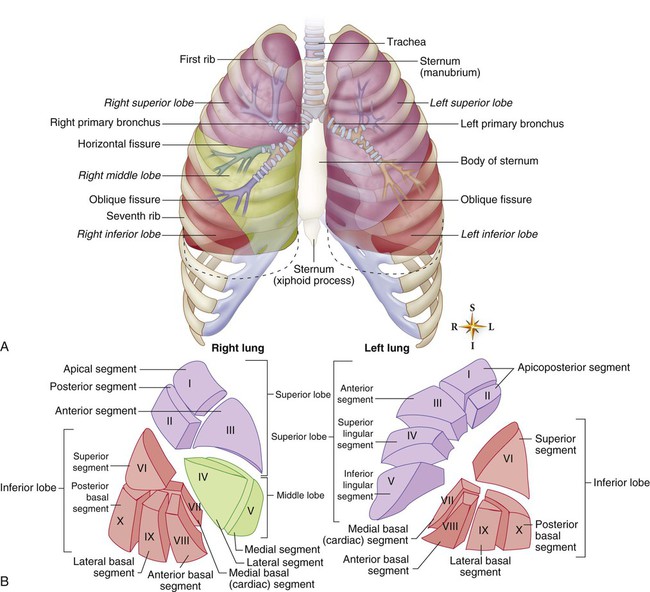
🔍 Hilum and Root of Lung
- Located on the mediastinal surface, containing:
- Bronchus (posteriorly placed on left, superiorly on right).
- Pulmonary arteries (superior).
- Pulmonary veins (inferior and anterior).
- Lymphatics and bronchial vessels.
- The pulmonary ligament extends below the hilum allowing expansion during respiration.
🧬 Bronchial Tree and Alveoli
- Trachea: Bifurcates at T4/5 (carina). Right bronchus is wider and more vertical — the common site for aspirated objects.
- Bronchi → Bronchioles → Alveolar ducts → Alveoli.
- About 300 million alveoli provide a surface area of ~90 m² for gas exchange.
- Type I pneumocytes: Thin squamous cells for diffusion.
- Type II pneumocytes: Secrete surfactant, reducing surface tension and preventing alveolar collapse (atelectasis).
- Alveolar macrophages: Phagocytose debris and pathogens.
🫧 Pleura and Pleural Cavities
- Visceral Pleura: Covers lungs, insensitive to pain.
- Parietal Pleura: Lines cavity, sensitive to pain (intercostal and phrenic nerves).
- Pleural Space: Thin film of fluid maintains negative pressure (−4 to −6 mmHg), enabling lung expansion.
- Clinical note: Air → pneumothorax; fluid → pleural effusion; pus → empyema.
⚙️ Mechanics of Breathing
- Inspiration: Diaphragm and external intercostals contract → thoracic volume ↑ → intrapulmonary pressure ↓.
- Expiration: Passive recoil of lungs and chest wall. Forced expiration recruits internal intercostals and abdominals.
- Accessory Muscles: SCM, scalenes, and pectoralis minor assist in laboured breathing.
🌬️ Gas Exchange & Transport
- Gas exchange occurs across a 0.4 µm alveolar–capillary membrane.
- O₂ diffusion: alveolus → capillary; CO₂ diffusion: capillary → alveolus.
- O₂ transport: 98% bound to haemoglobin; curve shifts right (Bohr effect) with ↑CO₂, ↓pH, ↑temp, ↑2,3-BPG.
- CO₂ transport: 70% bicarbonate, 20% carbamino-Hb, 10% dissolved.
🧠 Neural Control of Respiration
- Medulla: Generates basic rhythm (inspiratory and expiratory centres).
- Pons: Modulates transitions via pneumotaxic and apneustic centres.
- Chemoreceptors: Central (CO₂/pH in CSF) and peripheral (O₂ in carotid/aortic bodies).
- Stretch receptors: Prevent over-inflation (Hering–Breuer reflex).
💉 Pulmonary Circulation
- Pulmonary arteries: carry deoxygenated blood to alveoli (low pressure ~25/10 mmHg).
- Bronchial arteries: supply oxygenated blood to bronchial tissue.
- Hypoxic vasoconstriction: Diverts blood to better-ventilated alveoli — key adaptive mechanism but contributes to pulmonary hypertension in chronic hypoxia.
📊 Ventilation–Perfusion (V/Q) Matching
- Ideal ratio ≈ 0.8; varies by lung zone (apex > base).
- High V/Q: e.g. pulmonary embolism — ventilated but under-perfused.
- Low V/Q: e.g. pneumonia — perfused but under-ventilated.
- Both extremes cause hypoxaemia with normal or low CO₂.
📈 Lung Volumes and Spirometry
- Tidal Volume: 500 mL
- Inspiratory Reserve: 3 L
- Expiratory Reserve: 1.2 L
- Residual Volume: 1.2 L
- Vital Capacity: ~4.8 L; Total Lung Capacity: ~6 L
- FEV₁/FVC < 70%: Obstructive (COPD, asthma); preserved or ↑ in restrictive (fibrosis).
🩺 Clinical Correlations
- Pneumonia: Alveolar consolidation → ↓ gas exchange → ↑ A–a gradient.
- Asthma: Reversible bronchoconstriction and mucosal oedema.
- COPD: Emphysema (loss of alveolar walls) + chronic bronchitis (mucus hypersecretion).
- Pulmonary embolism: ↑ dead space, acute V/Q mismatch.
- Pneumothorax: Loss of negative intrapleural pressure → lung collapse.
🧩 Imaging and Procedures
- Chest X-ray: First-line for assessing lung fields, mediastinum, and pleura.
- CT Thorax: High-resolution for ILD, PE, and tumours.
- Ultrasound: For pleural effusion, diaphragm movement, and thoracentesis guidance.
- Bronchoscopy: Diagnostic and therapeutic airway visualisation.
📚 Clinical Pearls
- The Angle of Louis (T4/5) marks bifurcation of the trachea, start/end of aortic arch, and upper limit of pericardium.
- The right lung has 10 bronchopulmonary segments; the left has 8–9 — surgically resectable units.
- Phrenic nerve injury causes ipsilateral diaphragm paralysis (elevated hemidiaphragm on X-ray).
- Pleural effusion collects in the costodiaphragmatic recess, first seen on an upright chest X-ray.
🧠 Summary
The thoracic cavity and lungs together form a finely balanced pressure system. The structural integrity of the thoracic cage, neuromuscular control of the diaphragm, and efficiency of alveolar gas exchange together determine respiratory competence. An in-depth understanding of this region allows clinicians to interpret respiratory symptoms, imaging, and physiology with confidence — whether performing chest drainage, reading a CT, or managing ventilation in the ICU. 🌬️