Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Preterm labour
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Introduction to Obstetrics and Gynaecology |Female Reproductive Anatomy and Physiology |Basic Concepts of Pregnancy |Health Issues In Pregnancy |Risk assessment In Pregnancy |Anaemia In Pregnancy |Hypertension In Pregnancy |Diabetes In Pregnancy |Epilepsy In Pregnancy |Hyperemesis In Pregnancy |Obesity In Pregnancy |Prescribing in Pregnancy |Multiple Pregnancy |Preterm Labout |Management of Labour and Complications |Assessment of the newborn
The aim of preventing preterm birth is to improve the health of babies by prolonging pregnancy. Preterm birth, or delivery before 37 weeks’ gestation, affects 7.3% of pregnancies in the UK.1 Around 75% of these births result from spontaneous preterm labour. The best intervention for prevention of spontaneous preterm birth in women with risk factors is still unclear
Preterm Labour
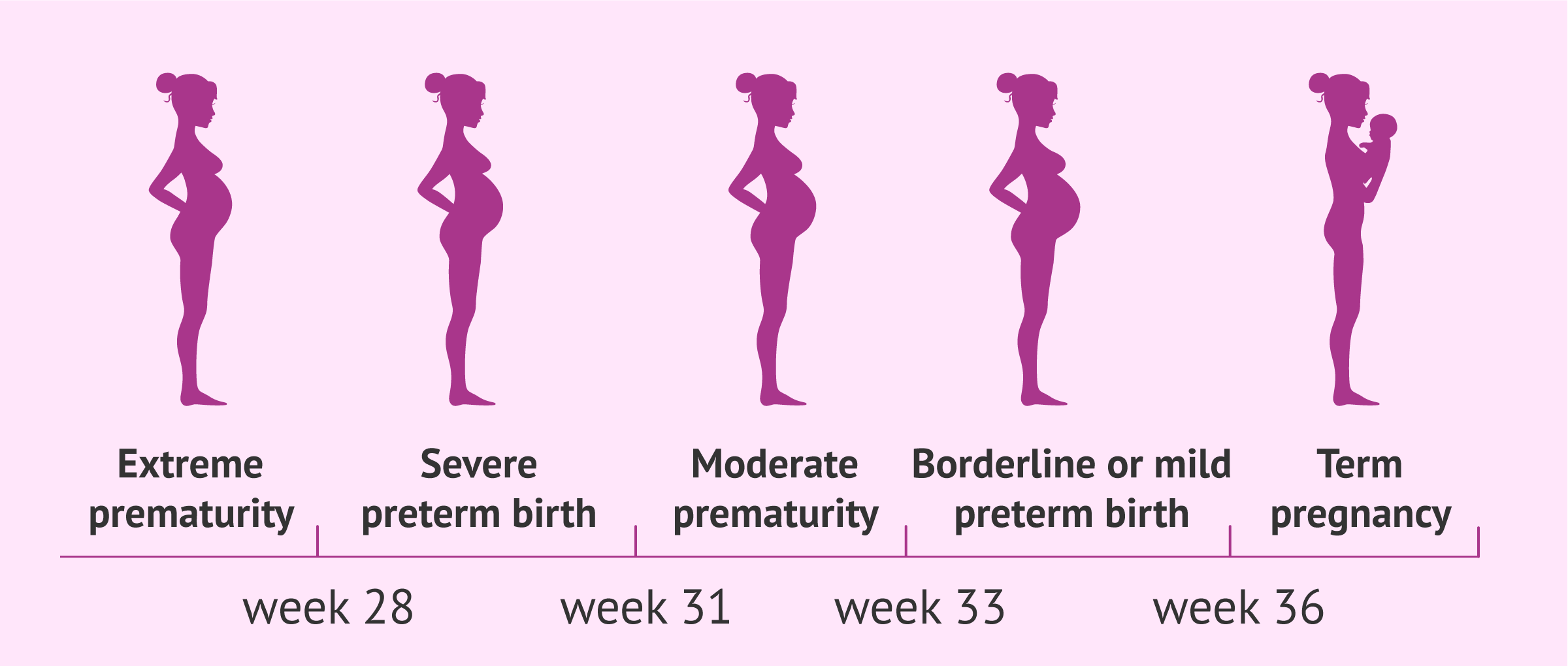
- Preterm labour refers to the onset of labour before 37 weeks of gestation, specifically between 24 and 37 weeks. It is a leading cause of neonatal morbidity and mortality, particularly when it occurs at earlier gestational ages.
- The majority of cases occur before 28 weeks, which significantly increases the risks for the infant. However, outcomes improve substantially for babies born after 32 weeks, with better survival rates and reduced complications.
Risks are History of mid-trimester loss, Preterm prelabour rupture of membranes in a previous pregnancy, Preterm birth in a previous pregnancy, History of cervical treatment for cervical intraepithelial neoplasia, short cervix (<25 mm) on transvaginal ultrasound examination
Aetiology
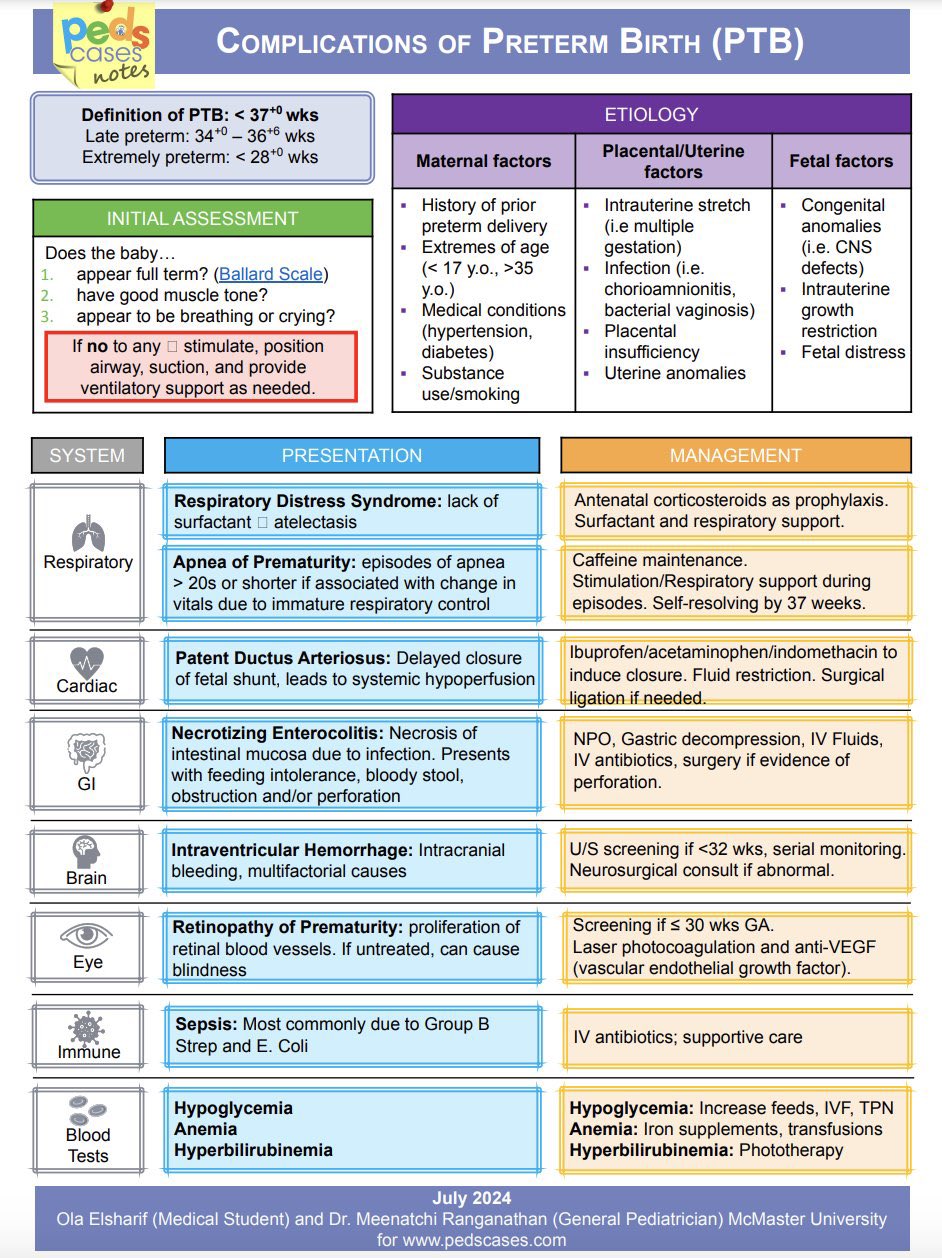
- Preterm labour poses a higher risk of infant mortality and serious neonatal complications, including respiratory distress syndrome, intraventricular haemorrhage, and necrotizing enterocolitis.
- Survivors of extreme prematurity (before 28 weeks) are more likely to experience long-term disabilities such as cerebral palsy, chronic lung disease, and neurodevelopmental delays affecting learning, vision, and hearing.
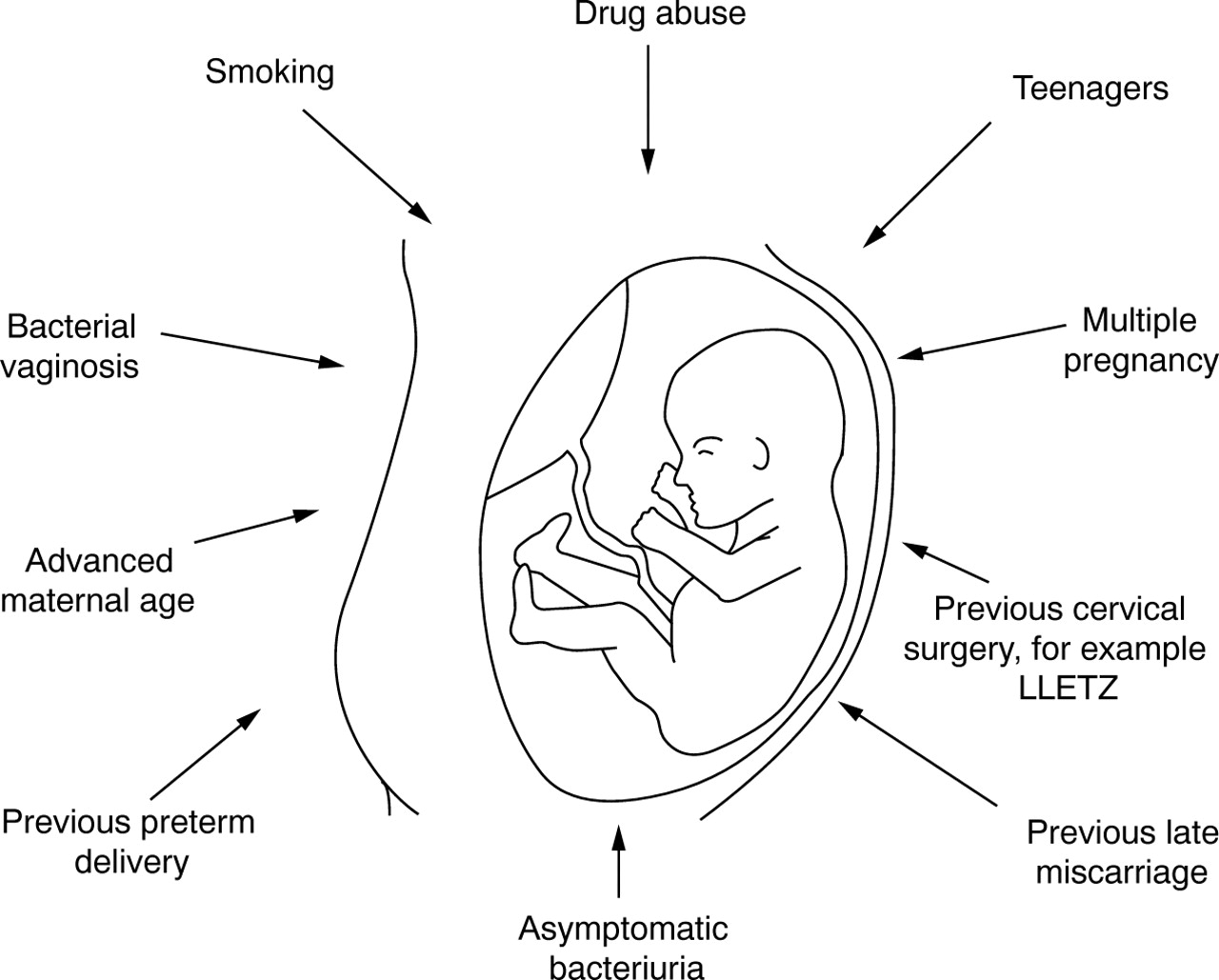
Risk Factors for Preterm Labour
- Maternal Factors:
- Low body mass index (BMI), maternal smoking, and poor socioeconomic conditions increase the likelihood of preterm birth.
- Psychosocial stressors, including domestic violence and lack of social support, have been associated with higher preterm labour rates.
- Women of Afro-Caribbean ethnicity are at a higher risk of preterm labour, likely due to a combination of genetic, environmental, and socio-economic factors.
- Obstetric Factors:
- History of preterm birth, multiple gestations (twins, triplets), and uterine abnormalities are key contributors to preterm labour.
Management of Preterm Labour
- Management of preterm labour aims to delay delivery long enough to optimize fetal outcomes, particularly by allowing time for corticosteroids to improve lung maturity and, where necessary, transfer to a specialist care centre. The primary goals include reducing the risks of severe neonatal complications and prolonging pregnancy if possible.
- Tocolytic Therapy:
- Tocolytics, such as β-agonists (e.g., Ritodrine, Salbutamol) or calcium channel blockers (e.g., nifedipine), may be used to suppress uterine contractions temporarily. While these agents can delay delivery for 24-48 hours, evidence suggests they do not significantly change long-term outcomes.
- Tocolytics provide a crucial window of opportunity to administer corticosteroids or transfer the mother to a tertiary care centre for optimal neonatal care.
- Antibiotic Prophylaxis:
- In cases of preterm premature rupture of membranes (PPROM), prophylactic antibiotics (e.g., erythromycin) are administered to reduce the risk of intrauterine infection and to prolong pregnancy.
- Infection can be both a cause and consequence of preterm labour; therefore, managing infection is critical to improving neonatal outcomes.
- Corticosteroids:
- Administering corticosteroids (e.g., betamethasone or dexamethasone) to the mother between 24 and 34 weeks reduces the risk of neonatal respiratory distress syndrome by accelerating fetal lung maturation.
- Corticosteroids also significantly lower the incidence of intraventricular haemorrhage and necrotizing enterocolitis, thus improving neonatal survival and long-term outcomes.
- Magnesium Sulfate for Neuroprotection:
- In pregnancies at risk of delivery before 32 weeks, magnesium sulfate is administered to provide neuroprotection and reduce the risk of cerebral palsy.
Management of Specific Causes
- Intrauterine Infection: Treat intrauterine infections with appropriate antibiotics to prevent maternal and neonatal complications. Infection is a common precipitant of preterm labour.
- Placental Abruption: Immediate obstetric evaluation is required in cases of placental abruption, as early delivery may be necessary to prevent fetal compromise or maternal haemorrhage.
- Elective Delivery: Preterm labour may require elective early delivery for maternal conditions such as preeclampsia or when there is fetal compromise (e.g., intrauterine growth restriction or abnormal Doppler studies).
- Cervical Incompetence: Women with a history of cervical incompetence may benefit from a cervical cerclage (surgical placement of a suture around the cervix) to prevent premature dilation. The suture is usually removed at 37 weeks or earlier if labour begins.
Further Management and Monitoring
- Cervical Assessment: Use transvaginal ultrasound to measure cervical length. A shortened cervix in the absence of dilation may indicate increased risk of preterm labour.
- Fetal Monitoring: Cardiotocography (CTG) or Doppler ultrasound can be used to monitor fetal heart rate and detect signs of fetal distress. Regular assessment of fetal growth is critical in managing preterm labour.
- Paediatric Team Involvement: Early involvement of the neonatal team is essential for planning neonatal resuscitation and transfer to a tertiary care unit if necessary.
- Corticosteroid Administration: Administer corticosteroids as two intramuscular injections, 12 hours apart. This reduces the risk of respiratory distress syndrome and other neonatal complications by enhancing fetal lung development.