Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Corneal Abrasion
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Episcleritis |Scleritis |Assessing a Red eye |Acute Angle Closure Glaucoma |Allergic and Infective Conjunctivitis |Anterior and Posterior Uveitis |Herpes simplex keratitis (HSK) |Acute Blepharitis |Corneal Abrasion
A corneal abrasion is a scratch or injury to the cornea, the clear, protective outer layer of the eye. This condition is usually caused by trauma, foreign bodies, or improper contact lens use. Superficial corneal injuries are non-penetrating injuries affecting the outermost layer of the cornea. Corneal abrasions are defects in the epithelial surface of the cornea — most heal within 1–2 days.
Causes of Corneal Abrasion
- Trauma :
- Accidental injury from fingernails, makeup brushes, or other objects.
- Blunt trauma to the eye.
- Foreign Bodies :
- Dust, sand, metal particles, or other small objects getting into the eye.
- Contact Lenses :
- Improper use or care of contact lenses, such as wearing them for too long or not cleaning them properly.
- Dry Eyes :
- Severe dryness causing the cornea to become more susceptible to abrasions.
- Eye Surgery :
- Post-surgical complications or accidental injury during surgery.
Symptoms of Corneal Abrasion
- Superficial corneal injuries typically present with sudden onset pain, discomfort or foreign body sensation of the eye and tearing.
- Severe pain and a gritty or foreign body sensation in the eye, Redness and tearing.
- Increased sensitivity to light (photophobia). Blurred vision or decreased visual acuity.
- Difficulty opening the eye due to pain.
Diagnosis: History Taking and Clinical Examination
- Detailed history to identify potential causes and associated symptoms.
- Ask what material the foreign body likely consists of, e.g. dirt, glass, metal or organic the mechanism of impact (hitting metal on metal is highly likely to cause a penetrating injury, whereas grinding or welding rarely do so)
- Exclude a penetrating eye injury as any penetration of the cornea or retained foreign body requires an urgent referral to an ophthalmologist for immediate consultation by phone.
- Discuss with senior staff if the foreign body is centrally located on the cornea (over the visual axis).
Comprehensive eye examination by an ophthalmologist or optometrist.
- Visual acuity: if not 6/6 then check with a pinhole.
- Slit lamp: assess for the size, site/s and nature of foreign body and the depth of penetration.
- Examine the cornea, anterior chamber, iris, pupil and lens for any distortion that may indicate ocular penetration and require urgent referral to an ophthalmologist.
- Evert the eyelids to exclude retained subtarsal foreign bodies and remove them if appropriate.
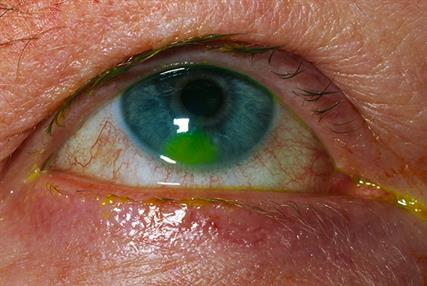
- Use fluorescein to exclude Seidel-positive corneal perforation and measure the size of the epithelial defect. Fluorescein should be used to stain the conjunctiva and cornea. An abrasion will fluoresce bright green with a cobalt-blue filter.
Indications for discussion with ophthalmology regarding urgency of referral include:
- Superficial corneal injury due to contact lens use.
- Recurrent erosion syndrome.
- Persistent or worsening symptoms after 24 hours.
- Rust rings that remain after removal of a metallic foreign body.
Immediate referral to the emergency eye service is required for:
- Suspected penetrating eye injury or intraocular foreign body.
- All high-velocity injuries (for example, due to hammering, chiselling, grinding, or lawn mowing), or injuries caused by sharp objects (for example, glass, knives, thorns, darts, or pencils) should be treated as penetrating injuries until proven otherwise.
- Chemical injuries:
- The affected eye should be immediately and copiously irrigated with normal saline or water for at least 20–30 minutes, and urgent ophthalmological assessment arranged.
- A foreign body that cannot be removed, or if the person is unable to tolerate examination.
- Other indications for immediate referral include:
- Any red flag symptom or sign for a serious eye condition such as severe pain, pupillary abnormalities, or a significant reduction in visual acuity.
- Hyphema (blood in the anterior chamber) or hypopyon (inflammatory exudate in the anterior chamber).
- Large or deep abrasions.
- Corneal opacities.
Treatment Options for Corneal Abrasion
- Medications :
- Lubricating eye drops or ointments to keep the eye moist and reduce discomfort.
- Antibiotic eye drops or ointments to prevent infection.
- Pain relief medications such as oral analgesics or topical NSAIDs.
- Protective Measures :
- Using an eye patch in some cases to keep the eye closed and facilitate healing.
- Wearing sunglasses to reduce light sensitivity and protect the eye from further injury.
- Follow-up Care :
- Regular follow-up visits to monitor healing and check for complications.
Complications of Untreated Corneal Abrasion
- Corneal infection or ulcer, leading to more severe damage and vision loss.
- Scarring of the cornea, causing permanent vision impairment.
- Chronic dry eye or recurrent corneal erosions.
Prevention and Management
- Loose superficial foreign bodies should be removed if the expertise and equipment are available in primary care.
- Analgesia and ocular lubricants should be offered for pain relief.
- The need for topical antibiotics such as chloramphenicol to prevent secondary infection should be considered.
- Wearing protective eyewear during activities that could result in eye injury.
- Proper use and care of contact lenses, following guidelines for cleaning and wear time.
- Avoiding rubbing the eyes, especially when there is a sensation of a foreign body.
- Advice should be given on suitable eye protection to prevent injury in the future. The person should be advised to avoid rubbing or touching the eye and contact lenses until the eye recovers.
- Follow up should be arranged in 24 hours to ensure the abrasion is healing as expected — the person should be advised to seek urgent medical review if symptoms worsen or new features develop in the interim.
Summary
Corneal abrasions are injuries to the cornea that can cause significant discomfort and potential complications if left untreated. Early diagnosis and appropriate treatment are crucial to prevent infection, scarring, and vision loss. Preventive measures, such as wearing protective eyewear and proper contact lens care, can help reduce the risk of corneal abrasions.