Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Human Herpesvirus 6A (HHV-6A)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
🧠 HHV-6 Encephalitis is a serious complication after stem cell transplants, often presenting with:
⚡ Hyponatraemia
| 🧩 Cognitive decline
| ⚠️ Seizures
| 📉 Memory loss
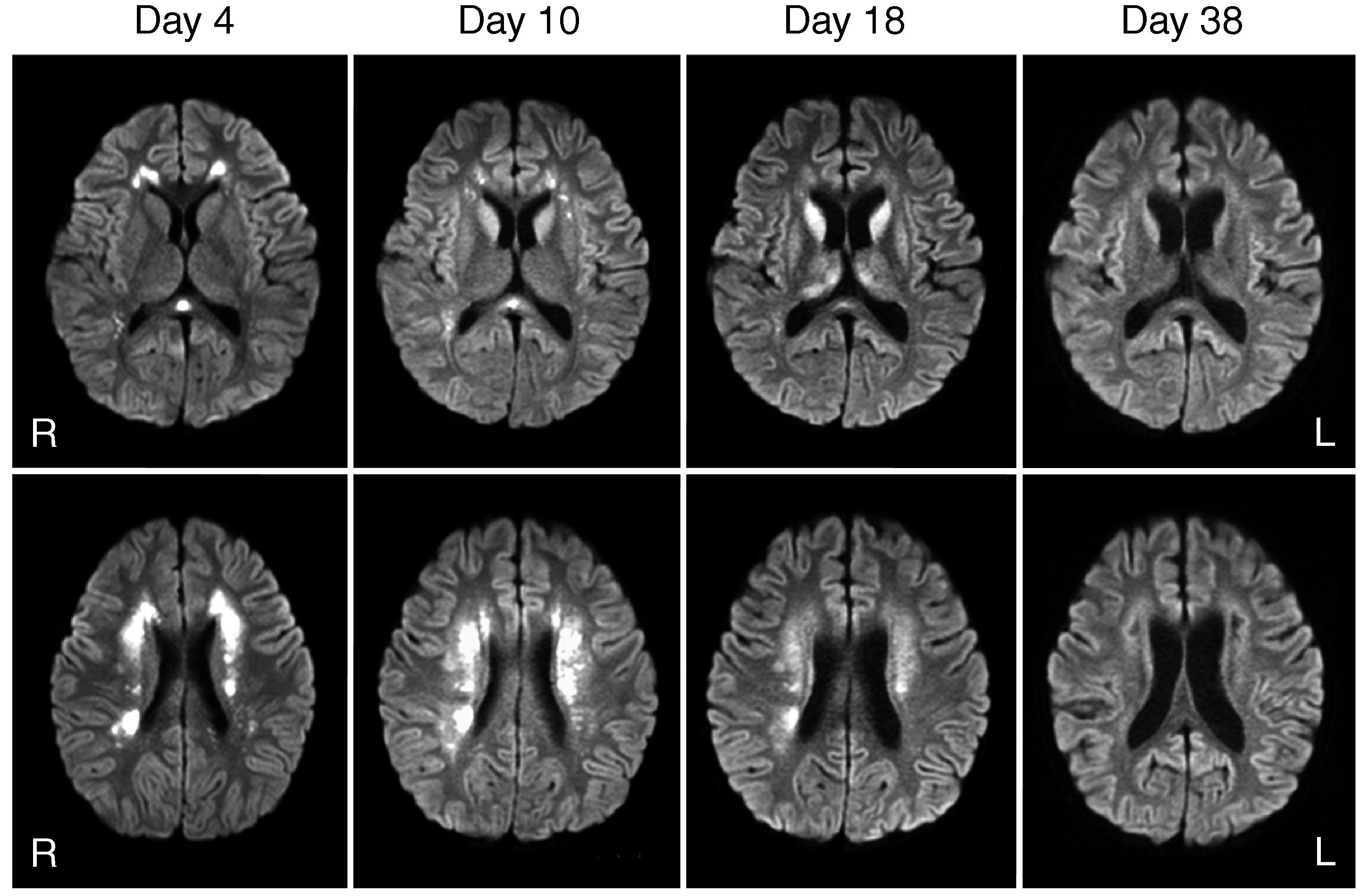
🧪 CSF & PCR are diagnostic gold standards. MRI (T2, FLAIR, DWI) typically shows hyperintensities in the medial temporal lobes, amygdala, and hippocampus.
💊 Treat with antivirals (foscarnet or ganciclovir). Prompt diagnosis is essential to prevent permanent neurological damage.
🔎 Overview
- HHV-6 = collective term for HHV-6A and HHV-6B.
- HHV-6A belongs to the Herpesviridae family (like HSV & CMV).
- HHV-6B commonly causes 🌸 roseola infantum in children.
- HHV-6A is less understood, often reactivates in immunocompromised patients.
- It is a double-stranded DNA virus, with T-lymphocytes as the main target.
📤 Transmission
- Worldwide, ubiquitous virus.
- HHV-6A: spread via close contact & saliva (exact routes unclear).
- Usually asymptomatic in healthy individuals.
- Reactivation occurs in immunosuppression ➝ drives complications.
🧬 Pathogenesis
- HHV-6A: infects CD4+ T cells, glial cells, macrophages, and epithelial cells. 🛑 Latency in monocytes/macrophages ➝ reactivation when immune defences fail. 🌀 Can disrupt immune balance → chronic inflammation, autoimmunity, or neurological disease.
- HHV-6B: causes roseola infantum (exanthema subitum) with fever + rash. ⚠️ Accounts for ~10–17% of febrile ED attendances in <36-month-olds.
🩺 Clinical Manifestations
- HHV-6A reactivation linked to:
- Neurological disease: encephalitis, MS associations, cognitive decline, seizures, SIADH.
- Chronic fatigue syndrome (possible role, under study).
- Immunosuppression in transplant patients.
- Worsening HIV progression by depleting CD4+ T cells.
- In healthy people ➝ often asymptomatic or mild flu-like illness.
🧪 Diagnosis
- PCR: most sensitive for viral DNA in blood/CSF.
- Serology: limited in distinguishing HHV-6A vs HHV-6B.
- Viral culture: rarely practical (needs high viral load).
- Tissue biopsy: brain biopsy in severe encephalitis cases.
- MRI: hyperintensity in medial temporal lobes (hippocampus + amygdala).
- EEG: temporal lobe epileptiform discharges may be seen.
🧒 Primary Infection
HHV-6B = roseola infantum → high fever + rash in infants. Complication: febrile seizures (most common). Rarely, acute encephalopathy.
💊 Treatment
- Most primary HHV-6 infections = self-limiting, resolve in 5–7 days.
- Complications: febrile seizures, encephalopathy due to neurotropic effect.
- For severe HHV-6A disease: use antivirals
- 🧪 Ganciclovir
- 🧪 Foscarnet
- 🧪 Cidofovir
- Supportive therapy: seizure control, management of raised ICP, fluid balance in SIADH.
⚠️ Complications
- Encephalitis: transplant recipients most at risk.
- Multiple sclerosis: association proposed, not proven.
- Chronic fatigue syndrome: under research as possible trigger.
- Long-term cognitive decline after encephalitis.
🛡️ Prevention
- No vaccine currently available.
- Strategies: close monitoring in immunocompromised patients (esp. transplant, HIV).
- Pre-emptive screening with PCR in post-transplant settings.
- Rapid initiation of antivirals when reactivation suspected.
📌 Conclusion
- HHV-6A is less understood than HHV-6B but is emerging as a key cause of CNS disease post-transplant.
- Diagnosis requires high suspicion + early PCR/MRI.
- Early antiviral therapy can prevent severe, irreversible neurological injury.
💡 Teaching Pearl: In transplant medicine, always consider HHV-6 encephalitis when you see: 📉 Memory loss + 🌙 confusion + ⚡ seizures + 🔬 hyponatraemia (SIADH). These are red flags for early MRI & PCR testing.