Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Penicillin Allergy
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Background
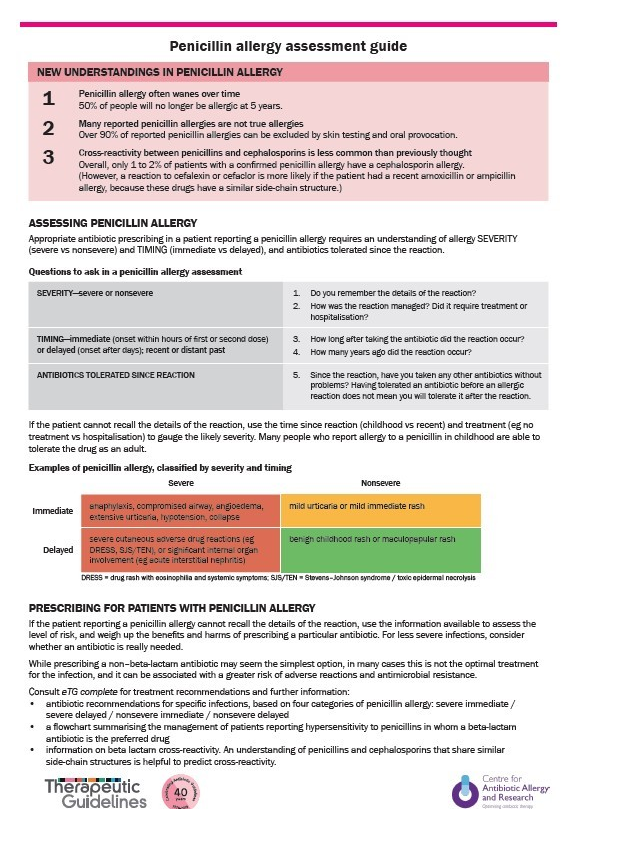
🧪 Penicillin allergy is often reported but rarely true: Around 10% of patients claim an allergy, yet <1% are truly allergic. Mislabeling leads to use of broader-spectrum, more toxic, and more expensive antibiotics, increasing risks of antimicrobial resistance and Clostridioides difficile infection.
- 🤔 Many “allergies” are side effects (e.g., nausea, vomiting) or viral rashes (e.g., amoxicillin + EBV infection) — not true allergies.
- ⌛ Sensitivity wanes: 50% lose penicillin allergy in 5 years, 80% in 10 years.
- 👶 Childhood penicillin “allergy” rarely persists into adulthood.
- 🔄 Cross-reactivity with cephalosporins is low (1–2%); most patients tolerate them.
- 🧪 Patients with mild, delayed reactions >10 years ago may be candidates for oral rechallenge under supervision.
- ✅ Careful assessment can often safely remove the penicillin allergy label.
- 💊 β-lactam allergies are the most common immune-mediated drug reactions encountered in clinical practice.
Taking a History of Penicillin Allergy
When a patient reports penicillin allergy, key questions include:
- 📜 Previous Reactions: Which antibiotics caused problems?
- 💊 Tolerated Antibiotics: Any β-lactams tolerated since?
- 🕒 Timing: How long ago did the reaction occur?
- ⚠️ Nature of Reaction: Was it diarrhoea, rash, swelling, breathing difficulty?
- 🎨 Rash Details: What type (maculopapular, urticarial, bullous)? Could it have been viral?
- ⏳ Onset: Minutes/hours (immediate IgE-mediated) vs days (delayed).
- 📍 Reason for antibiotic: Was it for a throat infection, skin infection, etc.?
- 🏥 Severity: Did it need hospitalisation or ICU?
- ✅ Resolution: Did it stop once the drug was discontinued?
- 📚 Sources: Ask patient, carers, GP, and check records.
Risk Stratification
- 🚨 Immediate reactions (minutes–hours, IgE-mediated): urticaria, angioedema, bronchospasm, hypotension, anaphylaxis.
- 📆 Delayed reactions (days–weeks, T-cell mediated): morbilliform rash, serum sickness, Stevens-Johnson syndrome.
- 🔑 Differentiation matters: delayed mild rashes often allow safe future use under supervision.
📝 Exam pearl: Only 1 in 10 patients labelled as penicillin allergic are truly allergic. Always clarify the history before defaulting to alternatives.
Assessment and Management
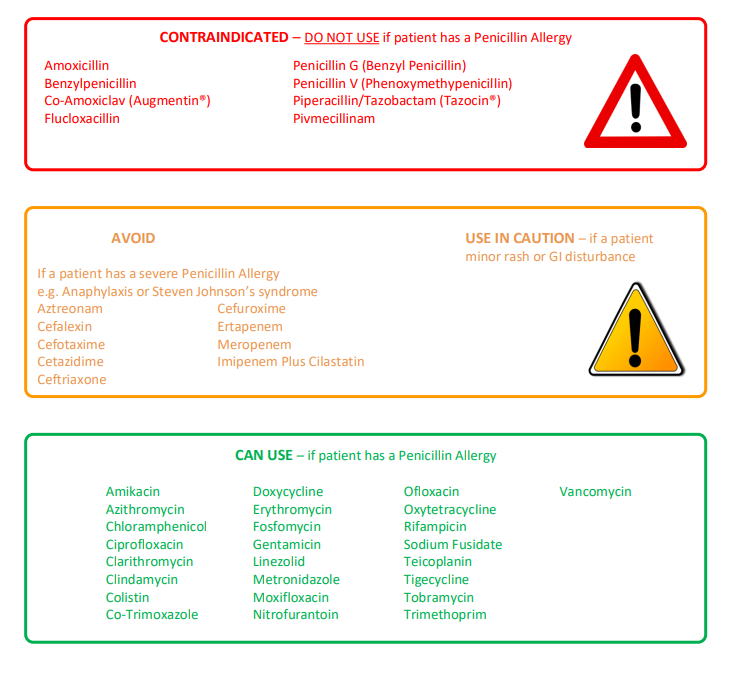
Understanding β-lactam classification helps guide safe prescribing:
- 🔴 Penicillins: Avoid in true allergy.
- 🟠 Other β-lactams (cephalosporins, carbapenems): Usually tolerated in mild allergy; caution in severe IgE-mediated cases.
- 🟢 Non-β-lactams: Always safe regardless of allergy history.
🌟 Delabelling strategies: Allergy testing (skin/IgE) and supervised oral challenge can safely remove false penicillin allergy labels, improving antibiotic stewardship.
Clinical Consequences of a False Allergy Label
- 💷 More expensive antibiotic prescriptions
- 🦠 Broader-spectrum antibiotics → antimicrobial resistance
- ⚠️ Higher rates of C. difficile infection
- ⏱️ Longer hospital stays & higher complication rates